Cardiac arrest is a sudden and life- threatening event where the heart stops pumping blood effectively, often leading to an immediate loss of consciousness, no pulse, and a sudden collapse.
This abrupt halt in cardiac function stops blood flow to the brain and vital organs. In the absence of immediate action like cardiopulmonary resuscitation (CPR), a person’s life can be lost in just a few minutes. Timely action, awareness of the warning signs, and basic knowledge of CPR procedures can significantly improve survival chances.
At Park Group of Hospitals, we are committed to saving lives through excellence in emergency cardiac arrest care. Our facilities are equipped with advanced technology and highly trained emergency teams at multiple locations, including Delhi, Gurugram (Sec-47, Palam Vihar, Sec-37 D), Faridabad, Sonipat, Panipat, Karnal, Ambala, Patiala, Mohali, Bathinda, Behror, and Jaipur. We believe in empowering communities through education, early intervention, and accessible expert care.
For immediate cardiac emergencies, contact Park’s 24x7 Emergency Services at: [99166 99166].
Your quick response can save a life.
Cardiac Arrest
Cardiac arrest refers to the sudden and unexpected loss of heart function, breathing, and consciousness. It typically results from an electrical malfunction in the heart, leading to an irregular heartbeat (arrhythmia). The heart’s pumping ability is disrupted, cutting off blood flow to the brain and other organs. If not treated immediately, the consequences of cardiac arrest can be life- threatening.
How Common Cardiac Arrest Is?
Cardiac arrest is a major public health concern and one of the leading causes of sudden death in India. According to multiple health studies and expert estimates, India reports over 700,000 cardiac arrest-related deaths annually. What makes this statistic even more alarming is that a significant percentage of these deaths occur outside of hospital environments — in homes, on roads, in offices, or public places — where access to immediate medical care is limited or absent.
Research indicates that the out-of-hospital cardiac arrest (OHCA) survival rate in India is less than 10 percent, primarily due to delays in recognition and response. Unlike countries with robust emergency systems and trained bystander networks, India faces challenges such as limited public awareness about cardiac arrest, lack of availability and use of automated external defibrillators (AEDs), and insufficient CPR training among the general population.
Another crucial factor is the delay in emergency medical services (EMS). In many Indian cities, especially tier 2 and 3 towns, ambulance response times remain high. Moreover, many people are unaware of the correct emergency numbers or hesitate to perform CPR due to lack of training or fear of legal implications.
Age and gender also influence the burden of cardiac arrest. It is more common in men, particularly those aged 45 and above, though younger adults and even adolescents with underlying heart conditions are not immune. Increasing prevalence of lifestyle-related conditions such as diabetes, hypertension, high cholesterol, and obesity has made the Indian population more vulnerable to sudden cardiac events.
In summary, India faces a rising number of cardiac arrest cases with low survival rates and limited public response. This highlights the urgent need for better awareness, CPR and AED training, and faster emergency services.
Types of Cardiac Arrest
Cardiac arrest can occur in various forms, depending on the underlying rhythm disturbances. The most common types include:
Ventricular Fibrillation (VF): A life-threatening arrhythmia where the heart's electrical signals become chaotic, causing the ventricles to quiver instead of pumping.
Ventricular Tachycardia (VT): A rapid heartbeat that begins in the heart’s lower chambers and can lead to VF or asystole.
Pulseless Electrical Activity (PEA): Electrical activity is detected, but the heart muscles fail to contract effectively.
Asystole is also known as flatline. This refers to the heart completely losing its natural electrical activity. This is the most severe and often irreversible form.
Cardiac Arrest Symptoms
Recognizing the symptoms of cardiac arrest promptly can mean the difference between life and death. Cardiac arrest usually strikes without warning, and in many cases, the affected person shows no prior signs. The classic and immediate signs of cardiac arrest include:
Sudden collapse without any prior indication
No detectable pulse or heartbeat
Absence of breathing or abnormal gasping
Loss of consciousness, where the person becomes unresponsive
These symptoms demand urgent medical attention. If bystanders notice any of these signs, they should begin cardiopulmonary resuscitation (CPR) immediately and call for emergency help without delay.
In some cases, however, people may experience warning symptoms in the hours or days leading up to a cardiac arrest. These can include:
A feeling of chest pressure or discomfort, often mistaken for indigestion or muscle soreness
Shortness of breath, even during rest or light activity
Irregular heartbeats or palpitations, which may feel like skipped beats or a racing heart
Unexplained fatigue or dizziness, sometimes accompanied by lightheadedness
These heart arrest symptoms may seem subtle at first, but ignoring them can be life-threatening. Especially in individuals with risk factors like heart disease, diabetes, or a history of high blood pressure, these early warning signs warrant immediate medical evaluation.
Timely recognition and action can prevent the condition from worsening and potentially save the person's life.
Causes of Cardiac Arrest
Cardiac arrest can result from a wide range of cardiac and non-cardiac causes, all of which disrupt the heart's normal electrical activity or pumping function. Identifying the root cause is essential for both emergency treatment and long-term prevention.
Common causes include:
Coronary Artery Disease (CAD): The most frequent cause of cardiac arrest, CAD occurs when arteries supplying blood to the heart become narrowed or blocked due to plaque buildup. This reduces oxygen supply and can lead to arrhythmias or a heart attack, triggering cardiac arrest.
Heart Attack (Myocardial Infarction): A heart attack can directly lead to cardiac arrest by damaging the heart muscle and causing sudden electrical instability. It is one of the most dangerous triggers of sudden cardiac events.
Electrolyte Imbalances: Imbalances in potassium, calcium, or magnesium, minerals critical for electrical signals in the heart, can lead to dangerous arrhythmias. These abnormal rhythms may escalate to cardiac arrest if not corrected promptly.
Cardiomyopathy: It is a condition marked by abnormal changes in the heart muscle, where it becomes overly thick, stiff, or increases in size. Over time, it weakens the heart’s ability to pump effectively and increases the risk of sudden arrhythmias and cardiac arrest.
Congenital Heart Defects: Structural heart issues present from birth may remain undetected until adolescence or adulthood. These abnormalities can interfere with electrical conduction and may result in cardiac arrest, especially during physical exertion.
Severe Trauma or Blood Loss: Major physical injuries, especially to the chest or head, or significant loss of blood, can suddenly impair heart function and lead to cardiac arrest.
Drug Overdose or Poisoning: Certain drugs particularly opioids, stimulants, or sedatives, can slow or stop the heart. Poisoning from chemicals or medications can also lead to fatal disruptions in heart rhythm.
Drowning or Electrocution: Both situations can disrupt the electrical activity of the heart, either through oxygen deprivation (in drowning) or direct electrical shock (in electrocution), resulting in sudden cardiac arrest.
Understanding the diverse causes of cardiac arrest is vital for prevention and prompt intervention. In many cases, early detection and proper management of the underlying condition can significantly reduce the risk of sudden cardiac events.
Risk Factors of Cardiac Arrest
Understanding your individual cardiac arrest risk factors is a critical step toward prevention and early intervention. While cardiac arrest can strike suddenly, often without warning, it is frequently associated with identifiable health and lifestyle risks. Addressing these risk factors can significantly reduce the likelihood of a cardiac emergency.
Major cardiac arrest risk factors include:
Family History of Sudden Cardiac Arrest or Heart Disease: Genetics play a significant role in heart health. If a close relative has experienced cardiac arrest, heart failure, or early-onset heart disease, your own risk increases.
Tobacco Use: Smoking damages blood vessels, reduces oxygen levels in the blood, and raises the risk of fatal arrhythmias. It is a major contributor to coronary artery disease, which can lead to cardiac arrest.
Excessive Alcohol Consumption: High alcohol intake can raise blood pressure, contribute to arrhythmias like atrial fibrillation, and weaken the heart muscle over time, all of which increase cardiac arrest risk.
Physical Inactivity: Sedentary lifestyles contribute to obesity, high blood pressure, and poor cardiovascular health. Regular exercise is key to maintaining a strong and efficient heart.
High Blood Pressure (Hypertension): Chronic hypertension causes the heart to work harder, potentially leading to thickened heart muscles, arrhythmias, and eventual cardiac failure or cardiac arrest.
High Cholesterol: Elevated LDL (bad cholesterol) levels can result in plaque buildup in arteries, increasing the risk of heart attack and the subsequent possibility of cardiac arrest.
Obesity: This is a key contributor to health problems such as elevated blood pressure and diabetes, both of which can increase the likelihood of cardiac arrest.
Type 2 Diabetes: Diabetes significantly raises the risk of both cardiac arrest and congestive heart failure due to its impact on blood vessels, nerve endings, and metabolic control.
Chronic Kidney Disease: Kidney dysfunction is closely associated with cardiovascular complications. The interplay between kidney and heart health is critical and often overlooked.
Previous Heart Attack or Diagnosed Cardiac Failure/Heart Failure: A history of myocardial infarction or existing heart failure severely compromises cardiac function. Such individuals face a higher chance of developing abnormal heart rhythms, which may lead to sudden cardiac arrest in the future.
By identifying and actively managing these risk factors through lifestyle changes, medications, and routine health screenings, individuals can lower their chances of experiencing cardiac arrest. Park Group of Hospitals offers comprehensive heart risk assessments and preventive cardiology services across all major locations to help you take control of your heart health.
Complications of Cardiac Arrest
A sudden cardiac arrest can quickly turn deadly if not managed within minutes. The immediate stop in blood flow impacts every organ system, with the brain being the most vulnerable to injury.
Brain Damage: Lack of oxygen (hypoxia) for even a few minutes can cause irreversible brain injury, affecting memory, cognition, and motor functions.
Multiple Organ Failure: Prolonged cardiac arrest can lead to the shutdown of vital organs like the kidneys, liver, and lungs, severely reducing survival chances.
Coma: Some survivors may fall into a coma due to extended oxygen deprivation, with recovery outcomes varying widely.
Post-Cardiac Arrest Syndrome: This includes a range of issues such as brain dysfunction, heart muscle damage, and a systemic inflammatory response, all of which complicate recovery.
Psychological Effects: Survivors often experience emotional and mental health challenges like anxiety, depression, or post-traumatic stress disorder (PTSD), requiring long-term support and rehabilitation.
Early resuscitation, advanced ICU care, and timely neurological assessment play a crucial role in minimizing these complications and improving quality of life post-recovery.
Cardiac Arrest Diagnosis
After a patient is stabilized, identifying the underlying cause of cardiac arrest is critical for preventing recurrence and guiding further treatment. Healthcare professionals use a combination of diagnostic tools to evaluate heart function and overall health:
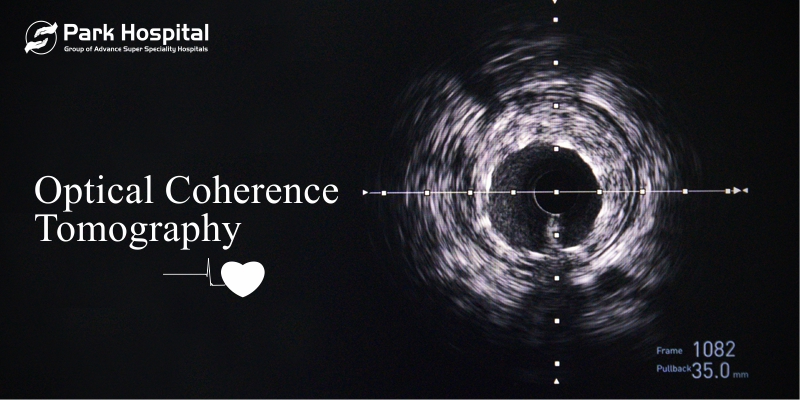
Electrocardiogram (ECG): A non-invasive test that monitors the heart’s electrical activity to detect arrhythmias or signs of previous heart attacks.
Blood Tests: Help identify elevated cardiac enzymes indicating heart muscle damage, along with checking for electrolyte imbalances that may trigger abnormal rhythms.
Echocardiogram: Uses ultrasound to visualize the heart’s structure and pumping efficiency, helping detect conditions like cardiomyopathy or valve disorders.
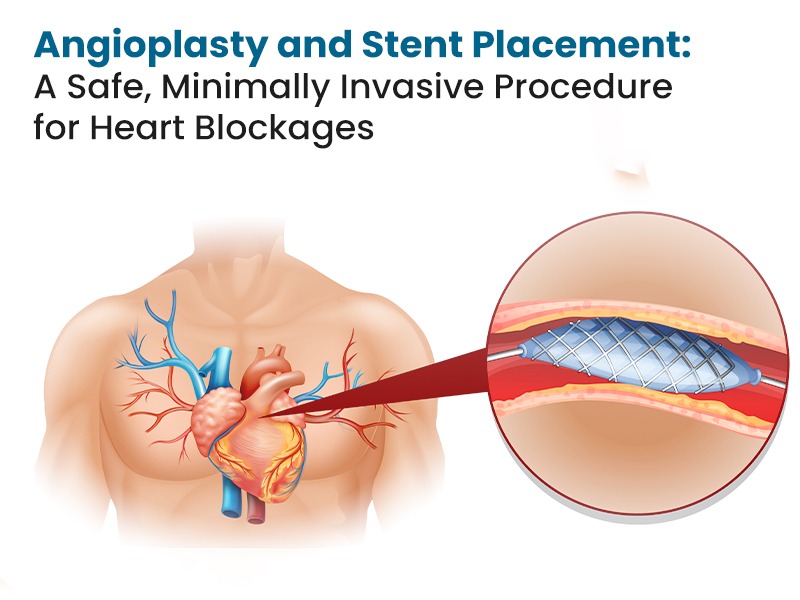
Cardiac Catheterization (Angiography): Involves inserting a thin tube into the heart to check for blockages in coronary arteries that may have caused the event.
CT or MRI Scans: Evaluate potential damage to the brain and other organs following cardiac arrest, especially if the patient was unresponsive for an extended period.
Prompt and thorough diagnosis is essential for tailoring treatment, monitoring recovery, and reducing the risk of another cardiac arrest.
Cardiac Arrest Treatment
Prompt and effective treatment is essential to increase survival chances after a cardiac arrest. The cardiopulmonary resuscitation procedure involves a coordinated series of emergency steps aimed at restoring heart function and minimizing organ damage:
Cardiopulmonary Resuscitation (CPR): Immediate, high-quality chest compressions help maintain blood flow to the brain and vital organs until medical help arrives.
Defibrillation: An AED (Automated External Defibrillator) delivers a controlled electric shock to restore a normal heart rhythm, especially in cases of ventricular fibrillation.
Advanced Life Support (ALS): Involves airway management, administration of emergency drugs (like epinephrine), and continuous monitoring of vital signs.
Post-Resuscitation Care: Intensive care includes therapeutic hypothermia (cooling the body to protect the brain), mechanical ventilation, and neurological evaluation to assess brain function and recovery.
At Park Group of Hospitals, we offer 24x7 emergency care and expert cardiac arrest management across all our centers, ensuring timely intervention with complete cardiopulmonary resuscitation procedures and critical care support.
Prevention of Cardiac Arrest
Many cases of cardiac arrest are preventable through lifestyle and medical interventions:
Monitor blood pressure and sugar levels
Regular cholesterol screening
Do moderate exercise for 20 minutes daily.
Eat heart-healthy foods low in salt and saturated fat
Avoid tobacco, alcohol, and recreational drugs
Practice stress-relief techniques such as yoga, mindfulness meditation, or therapy.
Attend regular health check-ups
At Park Group of Hospitals, we believe in proactive heart care. We offer:
Risk assessment programs
Nutrition and lifestyle counseling
CPR awareness programs and certified CPR training
BLS awareness drives
Preventive cardiology consultations in Delhi, Mohali, Jaipur, and other centers
Cardiac Arrest vs Heart Failure
Cardiac arrest and heart failure may sound similar, but they are very different in how they start and how they are treated.
Cardiac Arrest is a sudden stop in heart function due to electrical malfunction. Immediate intervention is critical.
Heart Failure (also known as cardiac failure) is a chronic condition where the heart cannot pump blood effectively, leading to gradual symptoms over time.
Understanding cardiac arrest vs heart failure can aid in timely recognition and appropriate treatment. While cardiac arrest requires emergency response, heart failure needs ongoing care with medication, lifestyle changes, and monitoring.
Difference Between Cardiac Arrest and Heart Failure
While cardiac arrest is an emergency requiring immediate action, heart failure also known as cardiac failure is a chronic condition that can be managed with long-term treatment. Understanding the difference between cardiac arrest and heart failure is crucial when it comes to seeking prompt and appropriate medical treatment.
Conclusion
Cardiac arrest is a life-threatening emergency that can strike without warning. Awareness of signs and risks, combined with the ability to perform CPR when needed, has the power to save someone’s life. The difference between cardiac arrest and heart failure lies in their nature and urgency, but both need proper medical attention.
Park Group of Hospitals is dedicated to offering expert cardiac arrest care, emergency services, and public CPR training. With facilities across 12 cities including Delhi, Jaipur, Mohali, and Bathinda, we ensure that life-saving heart care is never out of reach. Stay heart smart, stay informed, and take action because every second counts in a cardiac arrest emergency.
Frequently Asked Questions (FAQs)
Q1. What is cardiac arrest and how is it different from heart failure?
Cardiac arrest is an abrupt loss of heart function that requires emergency care, while heart failure is a long-term condition where the heart can't pump blood well. Cardiac arrest survival depends on fast CPR and defibrillation.
Q2. What are common cardiac arrest symptoms and heart arrest symptoms?
Sudden collapse, unresponsiveness, no breathing, and absence of a pulse are key symptoms. Other heart arrest symptoms can include chest pain, dizziness, or fatigue prior to the event.
Q3. What are the cardiac arrest risk factors?
A number of factors can increase your chances of developing heart disease or experiencing heart failure. These include having a genetic history of heart conditions, living with high blood pressure or diabetes, smoking habits, excessive body weight, and having suffered a previous heart attack or episodes of heart failure.
Q4. How do you perform CPR in a cardiac emergency?
Place both hands in the middle of the chest and deliver firm, rapid compressions, around 100 to 120 per minute. If you are trained, give rescue breaths between compressions. If AED is available nearby, use it as soon as possible.
Q5. Can cardiac arrest be prevented?
Yes, by adopting a heart-healthy lifestyle, managing health conditions like diabetes and hypertension, and getting regular check-ups.
Q6. Where can I get CPR training?
Organizations and hospitals, including Park Group of Hospitals, provide CPR training, CPR awareness programs, and basic life support sessions.
Q7. What is myocardial arrest?
Myocardial arrest, commonly referred to as cardiac arrest, is characterized by a sudden halt in the heart's activity, typically caused by an electrical disruption or direct muscle failure. It differs significantly from heart failure, which involves a gradual decline in cardiac function.
Q8. Who should be concerned about congestive heart failure?
Individuals with prior heart attacks, hypertension, diabetes, or valve diseases are at increased risk.