Coronary artery disease (CAD) is one of the leading causes of death worldwide and has become a major public health concern in India. It occurs due to plaque build-up in coronary arteries, makes it narrowed and blocked which creates obstruction in supply of oxygen-rich blood to the heart. This plaque consists of fat, cholesterol, calcium, and other substances in the blood. Over time, it causes the arteries to harden and narrow, reducing blood flow to the heart and leading to symptoms like chest pain (angina), shortness of breath, fatigue, or potentially a heart attack if left untreated.
A surge in coronary artery disease cases across India can be traced to factors like modern sedentary routines, unbalanced diets, high stress, and a notable rise in metabolic disorders like diabetes. Alarmingly, CAD is now affecting Indians at a younger age compared to global trends, underscoring the need for early detection and preventive care.
At Park Group of Hospitals, we are committed to tackling this growing crisis through comprehensive, patient-focused cardiac care. With advanced cardiac facilities across Delhi, Gurugram (Sec-47, Palam Vihar, Sec-37 D), Faridabad, Sonipat, Panipat, Karnal, Ambala, Patiala, Mohali, Bathinda, Behror, and Jaipur, our team of expert cardiologists and cardiac surgeons provides services ranging from early diagnosis and risk assessment to complex cardiac interventions and post-treatment rehabilitation.
Whether you have symptoms, a family history of heart disease, or simply want to take preventive steps, Park Group of Hospitals is here to support your journey toward a healthier heart and a better quality of life. For emergencies, our 24x7 cardiac response team can be reached at +91-99166 99166.
What is Coronary Artery Disease?
Coronary artery disease is a chronic, progressive condition that affects the arteries supplying blood to the heart muscle. These arteries, known as coronary arteries, are essential for delivering oxygen-rich blood that keeps the heart functioning properly. If the coronary arteries become narrowed or blocked, the heart may not receive the oxygen and nutrients it needs to pump blood efficiently. This reduction in blood flow is a defining feature of coronary artery disease.
The most common cause of coronary artery disease is a process called atherosclerosis, where plaque builds up inside the inner walls of the arteries. This plaque is made up of cholesterol, fatty substances, calcium, and cellular waste. Over time, the buildup hardens and narrows the arteries, restricting blood flow. In some cases, the plaque may rupture, leading to the formation of a blood clot that can completely block the artery and result in a heart attack.
Reduced or blocked blood flow due to CAD can cause a variety of symptoms and complications. One of the most common warning signs is chest pain or feeling of discomfort. This condition is also known as angina. It often occurs during emotional stress or physical activity, when the heart needs more oxygen. Other symptoms may include shortness of breath, fatigue, weakness, or even silent ischemia, where the reduced blood flow causes no noticeable symptoms but still damages the heart muscle.
If CAD is not detected and treated in time, it can lead to serious and potentially life-threatening complications such as heart attacks (myocardial infarction), arrhythmias (irregular heartbeat), heart failure, or sudden cardiac death. In many cases, coronary artery disease progresses silently over years before any symptoms appear, making regular heart health checkups essential, especially for individuals with known risk factors.
Types of Coronary Artery Disease
Coronary Artery Disease does not always present in the same way. It can develop gradually without symptoms or appear suddenly, depending on the level of blockage and how the heart responds to reduced blood flow. Understanding the different types of CAD is essential for early detection and effective treatment.
Stable Coronary Artery Disease
Stable CAD is the most common and predictable form of the disease. It occurs when a person experiences chest pain (angina) or discomfort during physical exertion, emotional stress, or after a heavy meal, which are situations where the heart requires more oxygen. The pain typically subsides with rest or nitroglycerin medication.
This condition is caused by partially blocked coronary arteries that restrict blood flow when demand increases. While not immediately life-threatening, it indicates significant artery narrowing and requires lifestyle changes and medical management to prevent progression.
Unstable Coronary Artery Disease
Unstable CAD is a medical emergency. It involves unexpected chest pain or feeling of discomfort, often at rest, and does not follow a predictable pattern. Unlike stable angina, which tends to follow a predictable pattern and responds to rest, this type can strike without warning and often does not improve with usual medications.
This type is usually caused by plaque rupture and blood clot formation, which may lead to a sudden blockage of blood flow to the heart. It significantly increases the risk of a heart attack (myocardial infarction) and requires immediate medical attention.
Silent Coronary Artery Disease (Silent Ischemia)
Silent CAD is especially dangerous because it develops without noticeable symptoms, yet causes real damage to the heart muscle. Many individuals with silent ischemia remain unaware of their condition until they suffer a heart attack or are diagnosed during tests for another issue.
This form is more common in individuals with diabetes, high blood pressure, older adults, or those with prior heart damage. Regular screening is essential for early detection in high-risk groups.
Variant Angina (Prinzmetal’s Angina)
Variant angina is a rare type of angina. It is caused by the sudden spasms in the coronary arteries which temporarily reduce or block blood flow to the heart, often leading to chest pain while at rest, usually at night or early morning.
The exact cause of these spasms is unclear, but factors may include cold exposure, stress, or certain medications. Although symptoms may resemble a heart attack, the cause is functional rather than structural. Prompt diagnosis is necessary to manage the condition effectively.
Coronary Artery Disease Causes
Coronary Artery Disease gradually develops over time. It results from cumulative damage to the coronary arteries due to various health conditions, lifestyle choices, and genetic factors. This damage restricts blood flow and can eventually lead to heart attacks, heart failure, and other serious cardiovascular complications.
Below are the major causes of CAD:
Atherosclerosis: The Root Cause
Atherosclerosis is the most common and direct cause of CAD. It occurs when plaque (a mix of fat, cholesterol, calcium, and cellular debris) builds up on the inner walls of the coronary arteries. With time, plaque buildup can cause the arteries to become stiff and narrow, limiting the amount of blood that reaches the heart muscle. The process is gradual and often silent. Many individuals may not show symptoms until the disease has advanced or a major event like a heart attack occurs. Atherosclerosis also increases the risk of blood clot formation, which can abruptly block an artery and trigger life-threatening complications.
High Cholesterol Levels
An imbalance in cholesterol levels is a key driver of atherosclerosis. An increase in low-density lipoprotein (LDL), often referred to as bad cholesterol, can lead to the accumulation of plaque in the arteries. Meanwhile, low levels of high-density lipoprotein (HDL), or "good" cholesterol, hinder the body’s ability to clear cholesterol from the bloodstream.
This imbalance significantly increases the risk of CAD, especially in individuals with poor dietary habits or a genetic predisposition to high cholesterol.
High Blood Pressure (Hypertension)
Hypertension causes mechanical damage to the inner lining of arteries. These small injuries make it easier for plaque to accumulate. The longer high blood pressure remains uncontrolled, the more damage it causes, leading to thickened and stiff arteries that are prone to narrowing. In addition, hypertension increases the heart’s workload, forcing it to pump harder, which accelerates the progression of CAD.
Smoking
Smoking is one of the major risk factors for CAD. The chemicals in tobacco smoke damage the endothelial lining of arteries, promote inflammation, raise LDL cholesterol, and lower HDL cholesterol. It also increases blood pressure and heart rate, making the cardiovascular system more vulnerable. Even secondhand smoke exposure increases the risk of CAD. This risk can be reduced effectively by quitting smoking.
Diabetes
Diabetes, especially type 2 diabetes, significantly raises the risk of CAD. Persistently high blood glucose levels damage blood vessels and nerves that control the heart, accelerating the process of atherosclerosis. People with diabetes often face additional risk factors such as obesity, hypertension, and high cholesterol, all of which further compound the threat to heart health.
Chronic Inflammation
Chronic inflammation contributes to the development and progression of atherosclerosis. Inflammatory responses from autoimmune diseases, infections, unhealthy diets, or smoking can destabilize plaque, making it more likely to rupture and cause a blood clot. Managing inflammation through lifestyle changes, medication, and control of underlying conditions is essential for reducing the risk of CAD.
Understanding these core causes of coronary artery disease is the first and most important step toward prevention and better heart health. Identifying and managing these risk factors early can significantly reduce the likelihood of developing severe cardiac complications later in life.
Coronary Artery Disease Risk Factors
Understanding the risk factors for coronary artery disease is essential for prevention and early intervention. These risk factors are generally divided into two categories: modifiable (factors you can change) and non-modifiable (factors you cannot control). Recognizing and addressing these risks, especially the modifiable ones, can significantly reduce your chances of developing CAD or slow its progression if already diagnosed.
Modifiable Risk Factors
These are lifestyle and health-related factors you can actively manage or improve with medical support and behavioral changes:
Smoking
A leading contributor to CAD, smoking damages blood vessels, lowers oxygen levels in the blood, raises blood pressure, and promotes plaque buildup. Quitting smoking significantly reduces your risk, regardless of age.Poor Diet
Diets high in saturated fats, trans fats, salt, and refined sugars increase cholesterol, promote inflammation, and elevate blood pressure. Adapting a heart-healthy diet rich in fruits, vegetables, whole grains, lean sources of protein, and good fats can play a vital role in improving your heart health.
Physical Inactivity
Lack of physical activity can lead to weight gain, increased blood sugar levels, elevated cholesterol, and high blood pressure. Regular physical activity improves heart strength, circulation, and blood sugar regulation.
Obesity and Overweight
Excess body weight, particularly abdominal fat, is linked to high cholesterol, hypertension, and type 2 diabetes. The risk of CAD can be reduced by maintaining a healthy weight.
High Cholesterol Levels
Elevated LDL (bad cholesterol) and low HDL (good cholesterol) accelerate plaque formation in arteries. A balanced lifestyle, supported by medical treatment when needed, plays a key role in managing cholesterol levels.
High Blood Pressure (Hypertension)
Persistent high blood pressure damages artery walls and promotes plaque buildup. It also puts extra strain on the heart, raising the risk of heart failure and stroke.
Diabetes (Type 1 & 2)
High blood glucose levels damage arteries and increase atherosclerosis risk. People with diabetes are two to four times more likely to develop CAD.
Excessive Alcohol Intake
Drinking too much can raise blood pressure, contribute to obesity, and harm heart muscle. If consumed, alcohol should be limited to recommended amounts.
Chronic Stress
Long-term stress can raise blood pressure, promote harmful habits like overeating or smoking, and increase stress hormones that damage arteries.
Non-Modifiable Risk Factors
These are factors you cannot change but should be aware of, especially if you have more than one:
Age
The risk of CAD increases with age. Men over 45 and women over 55 are more likely to develop heart disease due to cumulative risk exposure and vascular aging.
Family History of Heart Disease
A strong family history of early-onset heart disease (especially in parents or siblings) raises your risk. This genetic link is more dangerous when combined with poor lifestyle habits.
Gender
Men tend to develop CAD earlier than women. However, post-menopausal women are also at higher risk due to declining estrogen levels, which previously offered some cardiovascular protection.
Coronary Artery Disease Symptoms
The symptoms of Coronary Artery Disease (CAD) can vary greatly from person to person depending on the extent of arterial blockage, the presence of other health conditions, and individual pain thresholds. Some people may experience noticeable warning signs, while others may have no symptoms at all until a serious cardiac event occurs.
Recognizing these symptoms early can be life-saving, as it allows for timely diagnosis and treatment before severe complications develop.
Common Symptoms of Coronary Artery Disease
Chest Pain or Discomfort (Angina)
Chest pain or feeling discomfort, better known as angina, is one of the first warning signs of coronary artery disease. It may appear during physical activity or emotional stress and can feel like a heaviness, tightness, or pressure that sometimes radiates to the neck or arms.
Shortness of Breath
When the heart is unable to pump enough blood to meet the body’s oxygen needs, especially during exertion, it can result in difficulty breathing or a sense of breathlessness, even with mild activity or at rest.
Fatigue and Weakness
As the heart struggles to supply oxygen-rich blood, many people feel unusually tired or weak, especially during or after physical activity. This may suggest that the heart is not getting an adequate supply of blood.
Pain in Other Areas of the Body
Chest pain or feeling of discomfort is not observed in some cases. Instead, it may be experienced in areas like the neck, jaw, throat, upper stomach, shoulders, or even the back. This is particularly common among women, older adults, and people with diabetes.
Nausea, Indigestion, or Lightheadedness
Some people, especially women, may experience symptoms like nausea, vomiting, dizziness, or a sense of faintness instead of typical chest pain. These signs can be misleading but may still indicate serious heart disease.
Silent Ischemia: The Hidden Danger
One of the most dangerous aspects of coronary artery disease is that it can progress silently. Silent ischemia refers to a condition where the heart muscle does not receive enough oxygen, but the person experiences no obvious symptoms. Even without any noticeable discomfort, silent ischemia can quietly harm the heart and raise the chances of experiencing a sudden heart attack or cardiac arrest.
People with diabetes, older adults, and those with a previous history of heart disease are particularly vulnerable to silent CAD. That is why regular screening and cardiac checkups are essential, even if you feel healthy.
When to Seek Immediate Medical Attention
Immediately get medical help if you or someone nearby shows any of the following signs:
Sudden or severe chest pain
Pain spreading to the left arm, jaw, or back
Shortness of breath
Lightheadedness or fainting
A feeling of impending doom
These could be signs of a heart attack, and immediate medical attention can be life-saving.
Coronary Artery Disease Diagnosis
Timely and accurate diagnosis of coronary artery disease is essential to prevent serious complications such as heart attacks, arrhythmias, or heart failure. The diagnostic process involves a combination of clinical evaluations, non-invasive tests, and, when required, advanced imaging or invasive procedures.
Initial Assessment and Physical Examination
The process begins with a thorough review of your medical history, lifestyle habits, and risk factors such as high blood pressure, diabetes, smoking, or a family history of heart disease.
During the physical examination, the doctor may:
Check blood pressure, heart rate, and weight
Listen to heart and lung sounds
Look for signs such as leg swelling or irregular heartbeat
This step helps determine if further diagnostic tests are necessary.
Non-Invasive Diagnostic Tests
Non-invasive tests offer important information about heart function and potential arterial blockages without internal procedures.
Electrocardiogram (ECG or EKG): Evaluates how the heart's electrical system. It can detect irregular heart rhythms, previous heart attacks, and areas with reduced blood flow.
Stress Testing: Also known as a treadmill test, it evaluates how your heart responds to physical exertion. It helps identify symptoms like angina or ischemia that may not appear at rest.
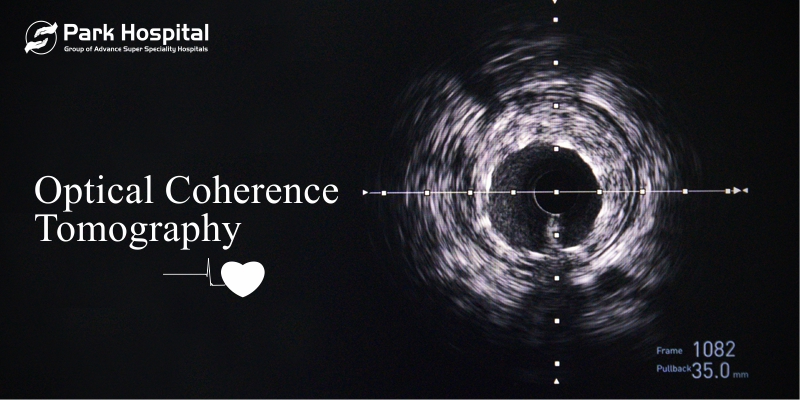
Echocardiogram: This is a type of ultrasound imaging that captures real-time visuals of how the heart looks and works, including its chambers, valves, and overall motion.
CT Coronary Angiography (CTCA): A high-resolution imaging test using contrast dye and CT scanning to visualize the coronary arteries. It helps detect plaque buildup and blockages early, without needing catheter insertion.
Invasive Diagnostic Procedures
If non-invasive tests are inconclusive or if a detailed view is needed, invasive testing may be recommended.
Coronary Angiography (Conventional Angiogram): This is the gold standard for diagnosing CAD. A thin catheter is carefully inserted through a blood vessel in the arm or groin region until it reaches the coronary artery. Once in place, a special contrast dye is introduced to make any blockages visible on X-ray images.
This procedure confirms the presence, location, and severity of arterial narrowing and helps guide treatment decisions such as angioplasty, stent placement, or bypass surgery.
Coronary Artery Disease Treatment
Coronary Artery Disease is a chronic condition that requires a combination of medical therapy, lifestyle changes, and sometimes surgical intervention. Treatment aims to improve blood flow to the heart, relieve symptoms, and prevent future complications such as heart attacks or heart failure.
Medications
Medications are often the first step in managing CAD, especially in mild to moderate cases. The goals are to lower cholesterol, control blood pressure, prevent blood clots, and reduce the heart’s workload.
Antiplatelet agents (e.g., aspirin): Help prevent blood clots in narrowed arteries, reducing the risk of heart attacks and strokes.
Statins: These drugs are effective in decreasing LDL (bad) cholesterol, which helps limit the accumulation of plaque and slows down the development of atherosclerosis in the blood vessels.
Beta-blockers: Reduce heart rate and blood pressure, easing chest pain and decreasing heart strain.
ACE inhibitors or ARBs: Help control high blood pressure and protect blood vessels.
Calcium channel blockers and nitrates: Help ease the tension in blood vessels, allowing better circulation and providing effective relief from angina.
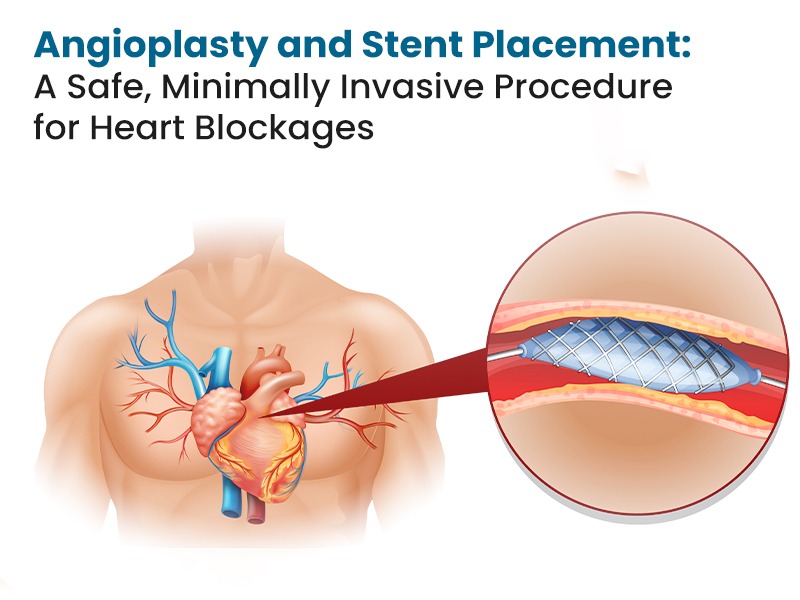
Surgical and Interventional Procedures
When medications are not enough or when blockages are severe, interventional or surgical options are considered to restore adequate blood flow.
Percutaneous Coronary Intervention (PCI): Also called angioplasty, a balloon is used to open blocked arteries, often followed by stent placement to keep the artery open.
Coronary Artery Bypass Grafting (CABG): Bypasses blocked arteries using grafts from other parts of the body, typically recommended for multiple or complex blockages.
Minimally Invasive Cardiac Surgery (MICS): Involves smaller incisions for selected patients, resulting in less pain and faster recovery compared to traditional open-heart surgery.
Cardiac Rehabilitation
Cardiac rehabilitation plays an important role for the patients in regaining strength following heart attack, angioplasty or bypass surgery. It supports long-term recovery by improving physical fitness and reducing the risk of future heart events.
A typical program includes:
Supervised exercise training
Nutritional counseling for heart-healthy eating
Stress management and emotional support
Education on medication adherence and symptom monitoring
This structured approach helps patients regain confidence and live a healthier life.
Lifestyle Changes for Long-Term Management
Lifestyle changes are the foundation of CAD treatment and vital for preventing disease progression.
Eat a heart-healthy diet: Emphasize fruits, vegetables, whole grains, legumes, lean proteins, and healthy fats.
Quit smoking: Tobacco use harms your blood vessels and significantly raises the chances of experiencing a heart attack. Quitting improves circulation and supports overall cardiovascular health.
Stay physically active: Incorporate moderate physical activity into your routine, aiming for about 20 minutes a day every week.
Keep your weight in check: Managing your weight supports overall heart health by preventing diabetes, hypertension, and poor cholesterol levels.
Manage stress: Practice relaxation techniques like meditation, deep breathing, or yoga to support emotional and cardiovascular well-being.
Coronary Artery Disease Complications
If left untreated or poorly managed, coronary artery disease can result in serious and potentially life-threatening complications. As plaque builds up in the coronary arteries, blood flow to the heart is gradually reduced, which can damage heart tissues and impair overall function.
Heart Attack (Myocardial Infarction)
A heart attack can occur when a blockage forms inside a coronary artery, usually after a plaque deposit ruptures, reducing the oxygen supply to the heart muscle.
Common symptoms include:
Severe chest pain or pressure
Sweating or nausea
Radiating pain in left arm, jaw or back
Shortness of breath
Immediate treatment can help reduce the extent of heart damage.
Heart Failure
Over time, coronary artery disease may impair the heart’s ability to function properly, resulting in heart failure. This happens when the heart can no longer pump enough blood to supply the body with the oxygen and nutrients it needs.
Symptoms may include:
Persistent shortness of breath
Unusual swelling around the feet, ankles, or lower legs
General fatigue
Weight gains due to fluid accumulation.
Heart failure requires continuous treatment with medication, lifestyle changes, and in some cases, implantable devices.
Arrhythmias (Irregular Heart Rhythms)
CAD-related damage to heart tissue can interfere with the heart’s electrical signals, causing arrhythmias.
Types include:
Atrial fibrillation
Ventricular tachycardia
Bradycardia (slow heart rate)
Some arrhythmias are harmless, while others may cause palpitations, fainting, or sudden collapse.
Sudden Cardiac Arrest
In severe cases, CAD may lead to sudden cardiac arrest, a sudden loss of heart function caused by electrical malfunction. Unlike a heart attack, which is caused by blocked blood flow, SCA results from a disrupted heartbeat and can lead to collapse within seconds Immediate cardiopulmonary resuscitation (CPR) and use of a defibrillator are essential to increase the chances of survival.
Stroke
Although CAD directly affects the heart, the same risk factors such as plaque buildup and clot formation can also increase the likelihood of an ischemic stroke. A small clot or fragment of plaque can move through the bloodstream and obstruct a vessel in the brain, potentially leading to reduced blood flow and resulting in brain injury. Managing blood pressure, cholesterol, and clotting risk is essential to lowering the chances of both heart attacks and strokes.
Coronary Artery Disease Prevention
Preventing Coronary Artery Disease (CAD) is possible with consistent, informed lifestyle choices and medical strategies. Since CAD develops gradually over time, early action plays a crucial role in reducing the risk of heart disease and its serious complications.
Eat a heart healthy diet Prioritize whole grains, fresh produce, legumes, and healthy oils like olive or mustard. Avoid processed foods, salt, sugar, and saturated fats. Add heart-healthy options like nuts, seeds, and fatty fish to support cardiovascular wellness.
Stay Physically Active: Aim for at least 20 minutes of moderate daily, such as brisk walking or cycling. It can help in maintaining a healthy weight, lowers blood pressure, and improves cholesterol levels.
Control Blood Pressure, Cholesterol & Diabetes: Routine checkups help monitor key health indicators, and proper treatment can protect your arteries and reduce the risk of coronary artery disease.
Manage Stress: Chronic stress can harm your heart health, so practicing meditation, deep breathing, or yoga can help you stay calm and protect your heart health.
Quit Smoking & Limit Alcohol: Tobacco use and excessive alcohol intake significantly increase the risk of CAD.
Conclusion: Take Control of Your Heart Health
Taking care of your heart begins with knowledge. Understanding the causes, recognizing the symptoms, and being aware of the treatment options for coronary artery disease empowers you to make informed decisions that protect your health and improve your quality of life.
CAD often progresses silently. But, acting promptly at an early stage can make a difference. Adopting heart-healthy habits such as eating a balanced diet, staying physically active, managing stress, avoiding tobacco, and monitoring blood pressure and cholesterol can help prevent serious complications.
Whether facing CAD or preventing it, consistent care makes all the difference. Timely diagnosis, appropriate treatment, and sustainable lifestyle changes can support a healthier, more active life.
Your heart works hard every day. Give it the care and attention it deserves through consistent, informed choices.
Frequently Asked Questions (FAQs)
What are the common symptoms of coronary artery disease?
Common symptoms of coronary artery disease include chest pain (angina), shortness of breath, fatigue, and discomfort in the shoulders, arms, neck, or jaw. Park Hospital emphasizes early recognition and diagnosis for effective treatment.
How is coronary artery disease diagnosed?
Diagnosis involves a physical examination, ECG, stress test, echocardiogram, and coronary angiography. Park Group of Hospitals is equipped with cutting-edge imaging technology to support accurate diagnosis and treatment.
Can coronary artery disease be cured?
While CAD cannot be fully cured, it can be effectively managed through medications, lifestyle changes, and surgical procedures.
Is cardiac rehabilitation necessary after treatment?
Yes, cardiac rehab plays a vital role in recovery, helping improve physical health, manage symptoms, and prevent recurrence.
How do I know if I am at risk for CAD?
You are at higher risk if you have a family history of heart disease, smoke, have high blood pressure, diabetes, or high cholesterol. Park Hospital provides full cardiac risk assessments to help you understand and manage your risk.